Fiber-optic Technology
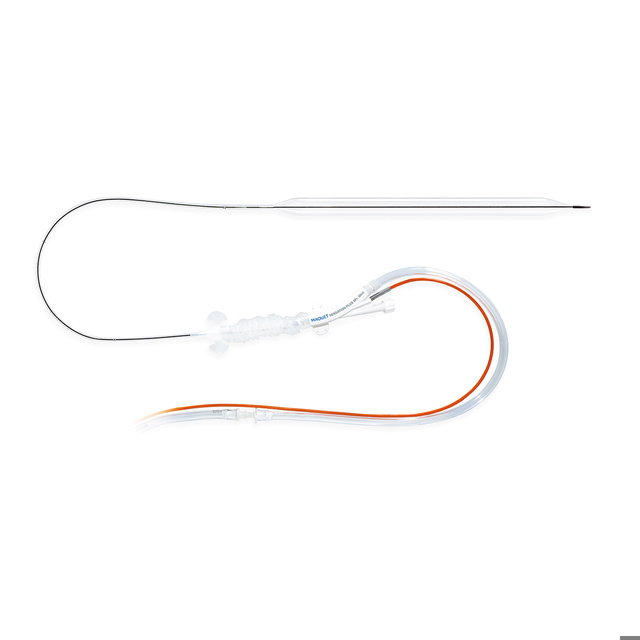
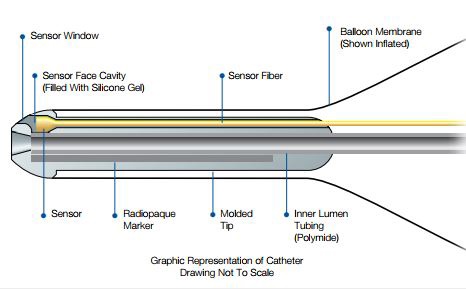
The Sensation Plus is the newest Getinge catheter that utilizes the benefits of fiber-optic technology. These benefits translate to faster initiation of therapy, easier patient management, crisp, clean arterial pressure waveform and automatic in vivo calibration.
- Faster time to therapy
- Automatic in vivo calibration
- Instantaneous signal transmission
- Crisp, clean arterial pressure waveform
- Low-level output capability
Greater Hemodynamic Support
Larger volume balloons like Sensation Plus displace more blood in the aorta during diastole, resulting in improved augmentation and unloading.*
- More blood volume displacement
- More diastolic augmentation
- More systolic unloading
- 40cc for patients 5'0" to 5'4" (152-162cm)
- 50cc for patients 5'4" (162cm) and taller.
Statlock® IAB Stabilization Device Included
Sensation Plus includes two complete, and ready-to-use Statlock® IAB Stabilization Devices that deliver sutureless securement benefits and comfort to you and your patients.
- Eliminates suture-securement needle sticks and suture-wound complications
- Patient comfort and safety
- Quick and easy application and removal
Visit our Academy – training and education designed to enhance your proficiency
For more information about our onsite events or remote trainings, you can also contact your local sales & service representative.