What is coronary artery disease?
Every year, millions of patients are diagnosed with some form of heart disease, and one of the most common is atherosclerosis.
At 32% cardiovascular disease was the leading cause of death worldwide.[1]
Atherosclerosis is commonly referred to as "hardening of the arteries". It refers to a gradual buildup of fatty deposits within the arteries that cause the arteries to become narrowed, or even blocked. When this process occurs in the coronary arteries, it is called coronary atherosclerosis or coronary artery disease (CAD).
When fatty deposits, called plaque, develop in the lining of these arteries, several things can happen:
- The lining of the artery becomes thicker and rougher
- Plaque buildup narrows the opening throughout the artery
- The narrowing makes it more difficult for blood to flow through the artery
- The heart has to work harder to pump blood
- The plaque can build up to a point where it completely blocks the flow of blood through the artery
- Or, the plaque may “rupture” or break free from the artery wall causing a partial or complete blockage of the artery – this may also prevent blood from being supplied to the heart muscle
If one or more arteries become blocked, heart tissue doesn’t get the blood supply it needs to function. The results can range from mild chest pain (angina) to a severe heart attack.
How to treat Coronary Artery Disease CAD?
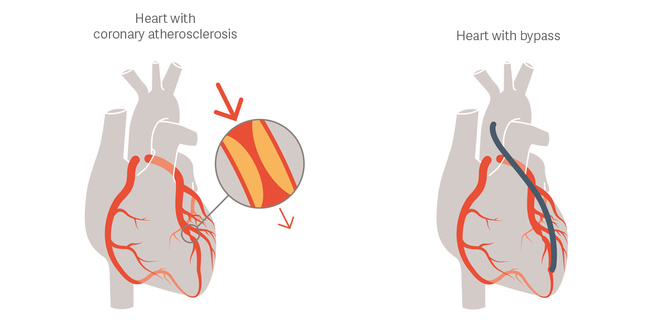
One of the treatment options for people that are diagnosed with coronary atherosclerosis is coronary artery bypass graft (CABG) surgery, a heart surgery procedure that restores blood flow.
For more than 50 years, coronary artery bypass graft (CABG) surgery has been the standard of care for revascularization of patients with coronary artery disease.[2]
Cardiovascular disease happens everywhere!
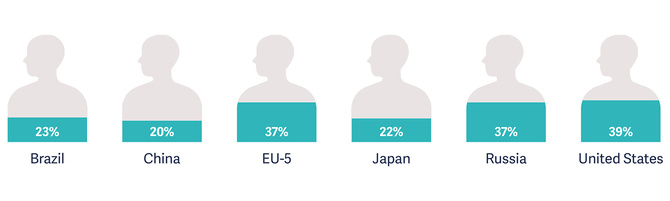
Prevalence of diagnosed cardiovascular conditions[3]

But the number of bypass anastomosis for heart revascularization procedures performed differ slightly.[4]
A new challenge for cardiac surgeon
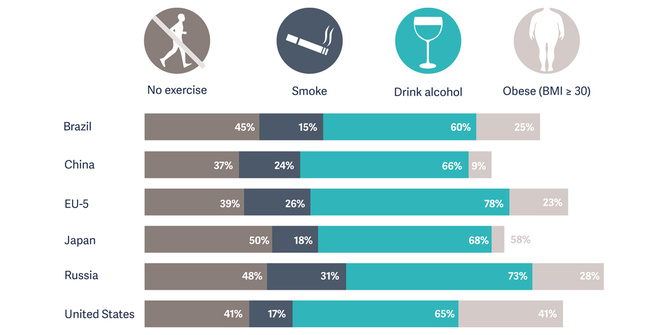
Today’s life styles changes and advancing age lead to higher CABG patient risk profile with multiple co-morbidities. This contributes to an increase in surgical complexity, perioperative complications and cost.[5]
More than 30% of patients presenting for CABG surgery are considered high-risk.[6] Some of these high-risk patients have predicted morbidity and mortality rates greater than 80%.[7]
Each step of the clinical pathway participate to a successful surgery and a good recovery
Pre-operative stabilization
Evidence-based medicine suggests that preemptive clinical protocols, which include advanced patient monitoring and a myocardial protective strategy, may help avoid procedural complications and shorten overall length of stay.[8] [9].
Intra-operative treatment
Optimize operative treatment can help minimize surgical complication. From the delivery of anesthesia, opting for beating heart surgery or approach to support a failing heart, using the right tool can help reduce complications, ventilation time and hospital costs.
Post-operative recovery
Low cardiac output syndrome and prolonged mechanical ventilation are common and costly post-operative complications following CABG surgery.[2],[10]

