Advanced technology to assess perfusion
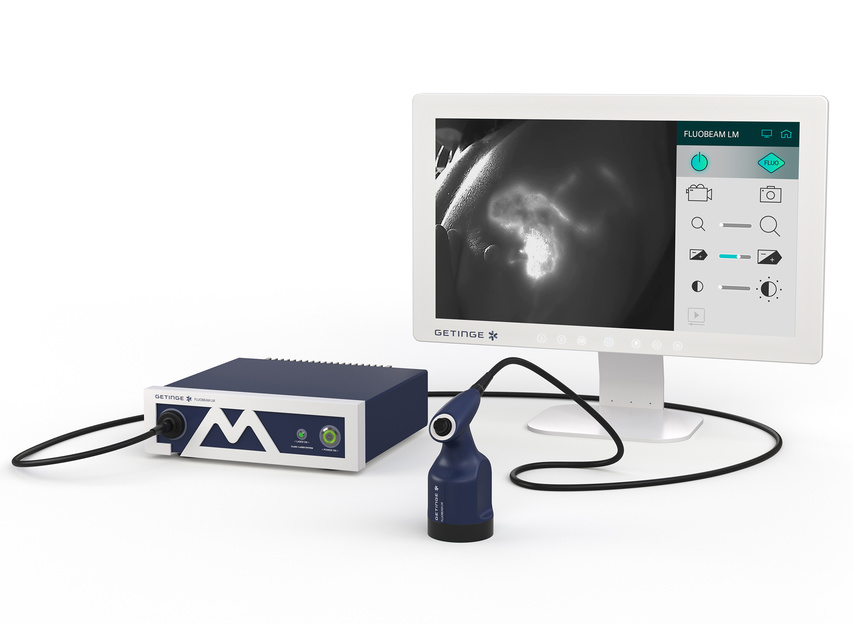
FLUOBEAM LM is dedicated to evaluating perfusion and lymphatic system. When used with Indocyanine Green (ICG), FLUOBEAM LM is an integrated fluorescence imaging solution that provides surgeons with a real-time image of tissue perfusion in fluorescence in the surgical field.

Excellence at your fingertips
FLUOBEAM LM is an integrated fluorescence imaging solution that provides the surgeon, during surgery, with information invisible to the naked eye such as tissue perfusion, lymphatic drainage status, or lymph node location. It helps the surgeon in his decision-making process in order to reduce the rate of complications.[1],[2],[3] Its ease of use and image processing functions makes it a major asset for surgeons.

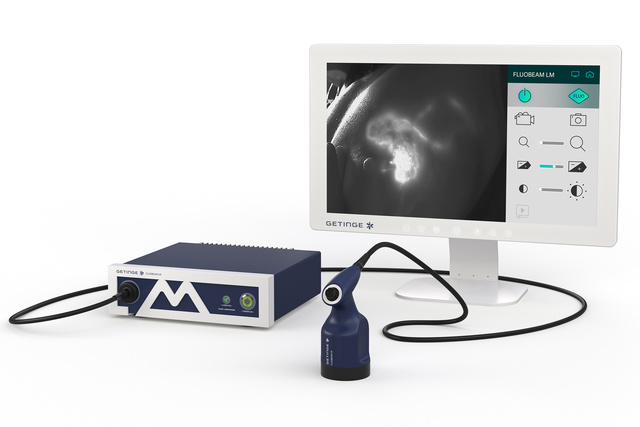
Ergonomics: a certain taste of freedom
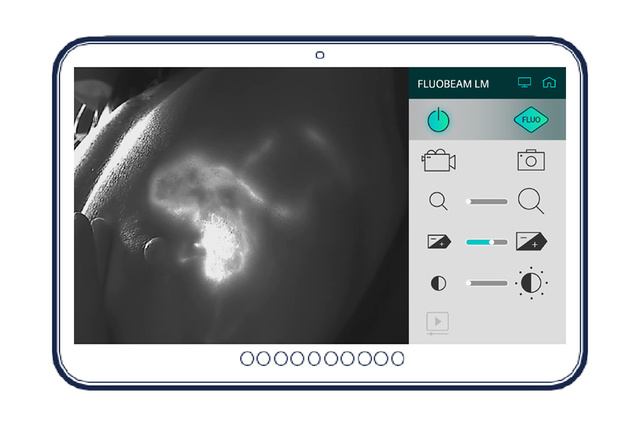
FLUOBEAM LM has been designed to be integrated in the surgical workflow. It offers the surgeon total autonomy during surgery, allowing him to control all acquisition and visualization parameters from the sterile area.

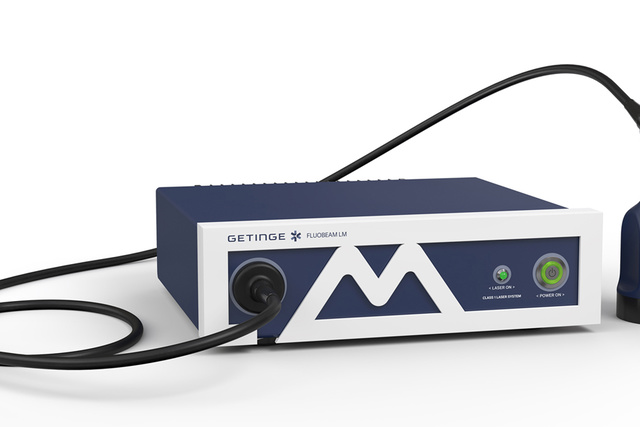
Safety: you won’t believe your eyes
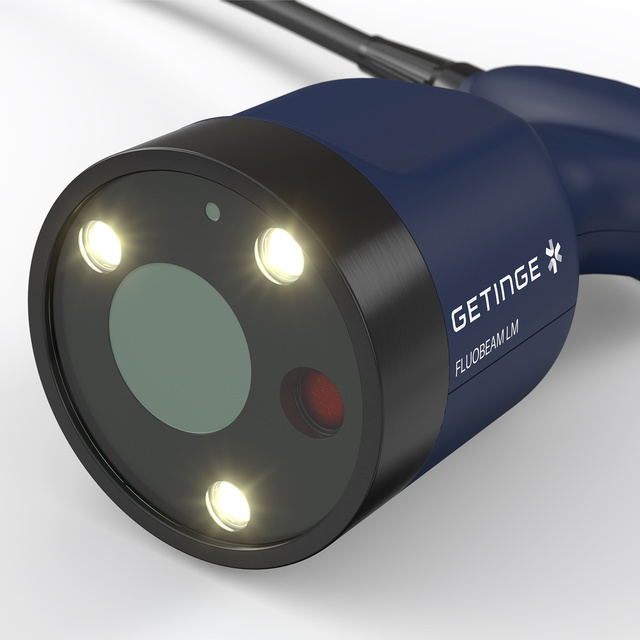
FLUOBEAM LM is an optically safe and ergonomic system. The camera combines safety and performance. Its optical head with a sensitive near-infrared camera excites the fluorescent agent with a class 1 laser, which is harmless to the eye even in direct vision.

Ergonomic and intuitive
The FLUOBEAM LM technology was developed to provide surgeons with a comfortable ergonomic camera and intuitive software during surgery.
Its joystick allows a fluid navigation in the software functionalities and offers the surgeon a total autonomy when using the device.
High performance and safety
FLUOBEAM LM has been designed to offer a high level of technical performance while ensuring surgeon and patient safety.
The power of its Class 1 laser and the quality of its optical filtering allow the surgeon to operate up to a working distance of 12 cm.
Automatic acquisition mode
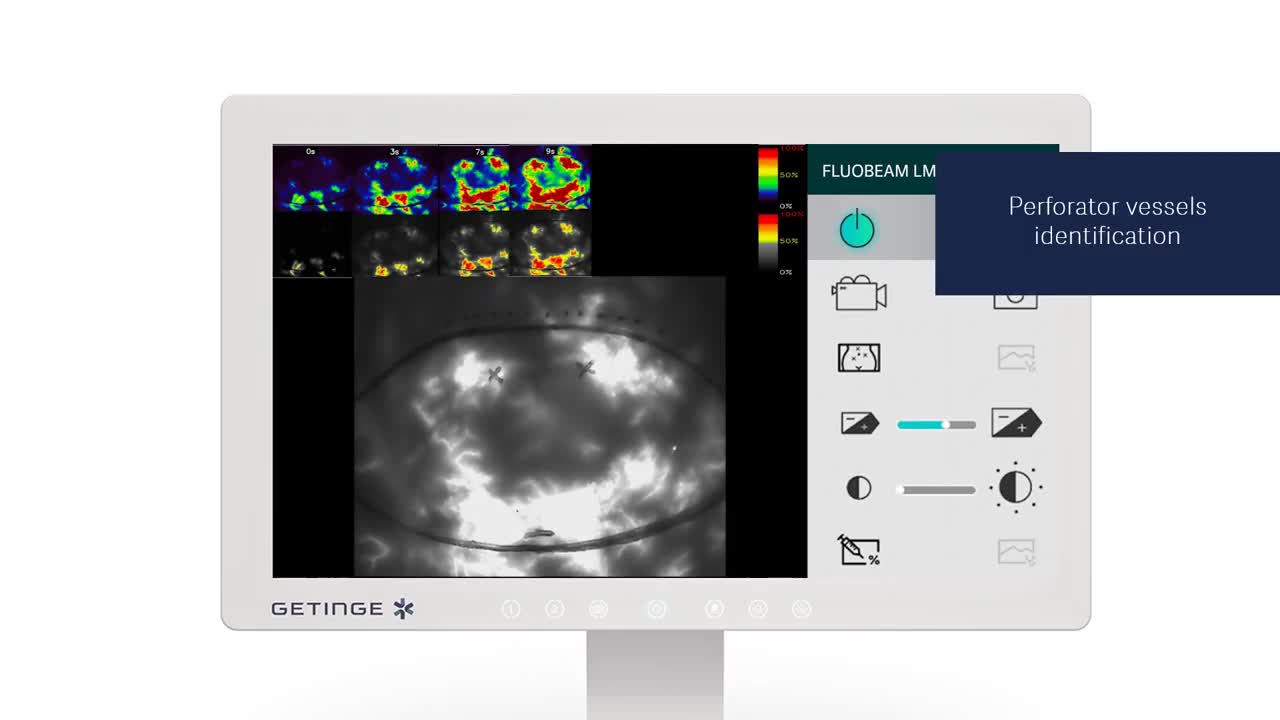
FLUOBEAM LM offers more than just images. Its integrated multi-indication software launches with a single click and automatically accesses dynamic information that is difficult to integrate with the naked eye.
The camera allows the surgeon to have direct and autonomous access to an analysis of the perfusion dynamics in the field, the location of the perforator vessels and the extent of their perfusion zone.
Related products

Perforator location in free flap reconstructive surgery
In free flap reconstructive surgery, FLUOBEAM LM helps to identify perforating vessels but also evaluate the quality of tissue perfusion in real time. This additional information helps limit postoperative complications such as total or partial tissue necrosis.
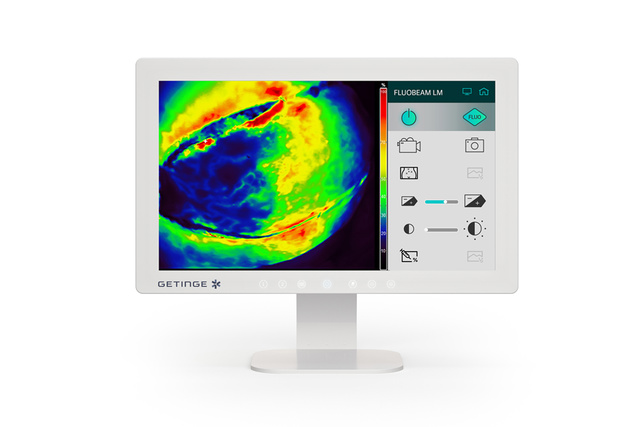
Evaluation of the quality of tissue perfusion
FLUOBEAM LM, used in combination with Indocyanine Green (ICG), is a fluorescence imaging solution that allows surgeons to assess the quality of tissue perfusion in real time.
In addition to real-time imaging, the relative quantification tool provides the surgeon with additional information that allows him to adjust his surgical procedure. This information will also be used to ensure follow-up and a post-operative evaluation adapted to each patient.

Visualization of lymphatic drainage
FLUOBEAM LM allows the surgeon to visualize the superficial lymphatic network of the limbs. The software offers a panoramic function to image an entire limb and better visualize the quality of the lymphatic drainage. In consultation or during a surgical operation, FLUOBEAM LM displays information in real time. It thus helps the surgeon to select the most appropriate treatment, for patients suffering from lymphedema.
An indication-oriented software
The integrated FLUOSOFT LM imaging software offers acquisition modes by type of indication; it automatically adapts to the visualization conditions: high sensitivity for low fluorescence applications, pseudocolorization with relative quantification to assess perfusion, automatic tool to help in perforator vessels identification before flap dissection, panoramic imaging of lymphatic drainage. This approach, associated with proven acquisition protocols, avoids handling errors and ensures high reliability of results.[1],[4]
Fluorescence imaging brings benefits in
Plastic and Reconstructive surgery
- Help in identifying intraoperatively perforator vessels and perforator angiosome
- Real-time intraoperative tissue perfusion assessment
- More precise flap design according to the perfused areas
- Relative quantification tool (additional information to improve the specificity of the method)
- Early identification of complications [4],[5]
- Postoperative monitoring
Axillary sentinel lymph node biopsy
- High detection rate (similar to radioisotope)
- Simple patient care pathway (one injection only on the day of surgery)
- Direct visualization (lymphatic drainage and SLN)
- No need for radioactive marker injection
Lymphatic drainage visualization
- Early identification and localization of lymphatic drainage deficiencies to establish appropriate treatment
- Accurate location of lymph nodes during lymph node transfer surgery
- Reverse mapping capability
- Accurate visualization of functional lymphatic vessels before lymphaticovenous anastomosis (LVA)
- Post-treatment monitoring
Fluorescence imaging in plastic and reconstructive surgery
Plastic and reconstructive surgeries require precise assessment of tissue perfusion quality to prevent partial necrosis. Indocyanine Green (ICG) fluorescence angiography offers reliable verification of tissue perfusion and identification of at-risk areas. FLUOBEAM LM facilitates real-time visualization of ICG flow, distribution, and accumulation on a screen during surgery, aiding in visualizing blood flow.
Breast reconstruction
FLUOBEAM LM allows the surgeon to evaluate in real time the quality of tissue perfusion (flaps or skin after mastectomy with preservation of the skin flap) and to adapt the surgical procedure to minimize the risks of complications.
During a reconstruction procedure, with the use of an autologous flap (free or pedicled), it is essential to ensure good tissue perfusion to avoid postoperative complications, such as partial or fat necrosis.

Fluorescence imaging in lymphatic surgery
In lymphatic surgery, it is essential to precisely locate functional lymphatic vessels. During consultation and surgery FLUOBEAM LM is used to image in real time the quality of the lymphatic network.
Lymphatic surgery
Observation of lymphatic vessels
In medical consultation, FLUOBEAM LM can be used for real-time imaging of functional superficial lymphatic vessels. It helps in the early diagnosis of lymphedema, in the choice of treatment (surgical or medical), and in the postoperative follow-up.
In surgery, FLUOBEAM LM can be used to identify before and during surgery the functional lymphatic vessels that will be used for a lymphaticovenous anastomosis (LVA). In addition, FLUOBEAM LM can be used in “reverse mapping” to map and preserve lymphatic drainage during lymph node surgery and can also be used for postoperative follow-up.
Sentinel lymph node biopsy
The sentinel lymph node is the first lymph node where cancer cells are most likely to migrate from the primary tumor. The sentinel node technique involves detecting this node, removing it and having it analyzed.
Fluorescence imaging and Indocyanine Green (ICG) have been recently introduced in the clinic as an alternative for surgical guidance. FLUOBEAM LM allows visualization of superficial lymphatic drainage and detection of the sentinel lymph node after incision, for different tumor types.
Marketing Sales - Brochures
-
Advanced technology to access perfusion
Visit our Academy – training and education designed to enhance your proficiency
For more information about our onsite events or remote trainings, you can also contact your local sales & service representative.