Challenge:
Optimizing volumetric treatment for ARDS patients
The life of the critically ill patient depends on the right decision for the next therapeutic step. With ARDS this becomes even more critical because the injured lung has an increased lung permeability resulting in pulmonary edema. The need for an early clear picture of the patient’s hemodynamic status in order to apply appropriate therapy is essential. The speed of therapy influences outcome.
Can we quantify pulmonary edema?
The last 2 decades have witnessed the introduction and evolution of the transpulmonary thermodilution (TPTD) technique. [1] This enables the quantification of pulmonary edema by extravascular lung water index (ELWI) and pulmonary vascular permeability index (PVPI). PVPI enables differential diagnosis of the origin of pulmonary edema: cardiogenic or permeability induced. ELWI and PVPI may be used as criteria indicating the risk of fluid administration. [2]
Extravascular lung water is an accumulation of fluid in the interstitium of the lung tissue and / or the alveoli. Pulmonary vascular permeability index (PVPI) is an indirect reflection of the integrity of the alveolo-capillary barrier.
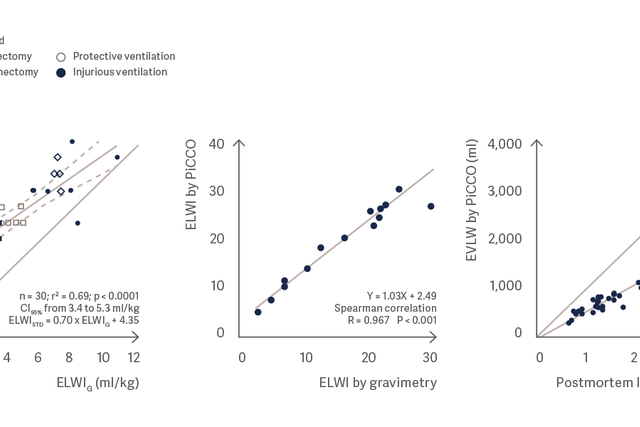
The lung water measurement using PiCCO correlates very well with the gravimetric lung water measurement and the post mortem lung weight. [3], [4], [5]
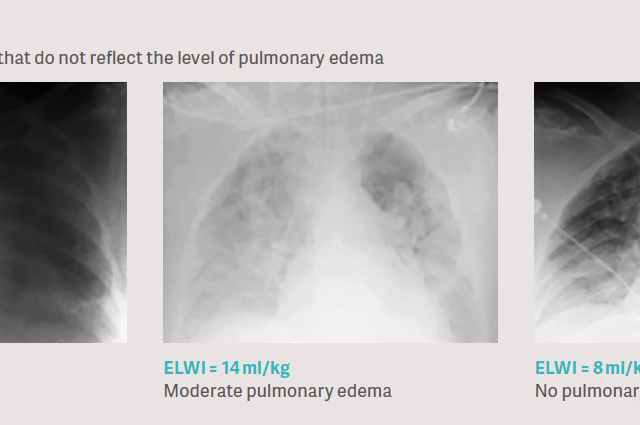
Clinical issue: Chest x-rays do not reliably reflect the level of pulmonary edema
The usual clinical approach to assess pulmonary edema is the evaluation of a chest x-ray. This is very challenging as the chest x-ray is a density measurement, influenced by all compartments in the chest like bones, muscles, tissue layers, blood, blood vessels, air, tissue edema, pleural effusion and possibly also pulmonary edema. Thus, in clinical studies it was demonstrated that chest x-ray evaluation for pulmonary edema is very inaccurate when comparing it to the direct quantification by transpulmonary thermodilution. [6], [7], [8].
Cardiogenic or permeability pulmonary edema?
PVPI is an indirect reflection of the integrity of the alveolo-capillary
barrier. It is calculated from the relation between EWLI and Pulmonary Blood Volume (PBV), the ratio of the fluid volume that is out of the vessels over the fluid volume that remains in the vessels. [9]
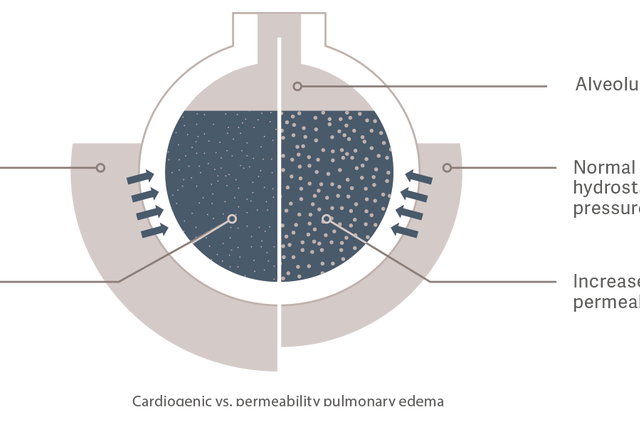
Cardiogenic pulmonary edema
Hydrostatic pressure increases as a result of intravascular fluid overload.
This causes fluids to leak into the extravascular space.
Permeability pulmonary edema
Vascular permeability is increased by an inflammatory reaction caused for example, by sepsis. This leads to the increased transfer of fluids, electrolytes
and proteins from the intravascular to the extravascular space, even
with a normal to low intravascular fluid status and hydrostatic pressure.
Interaction of ELWI and PVPI is of clinical benefit
The need to identify and quantify pulmonary edema in complex syndromes such as ARDS can influence outcomes. Pulmonary edema accumulation impairs respiratory gas exchange, resulting in respiratory distress. The parameters ELWI and PVPI can be used to sensitively quantify pulmonary edema at the bedside. It also allows the evaluation of the severity of ARDS.[2]
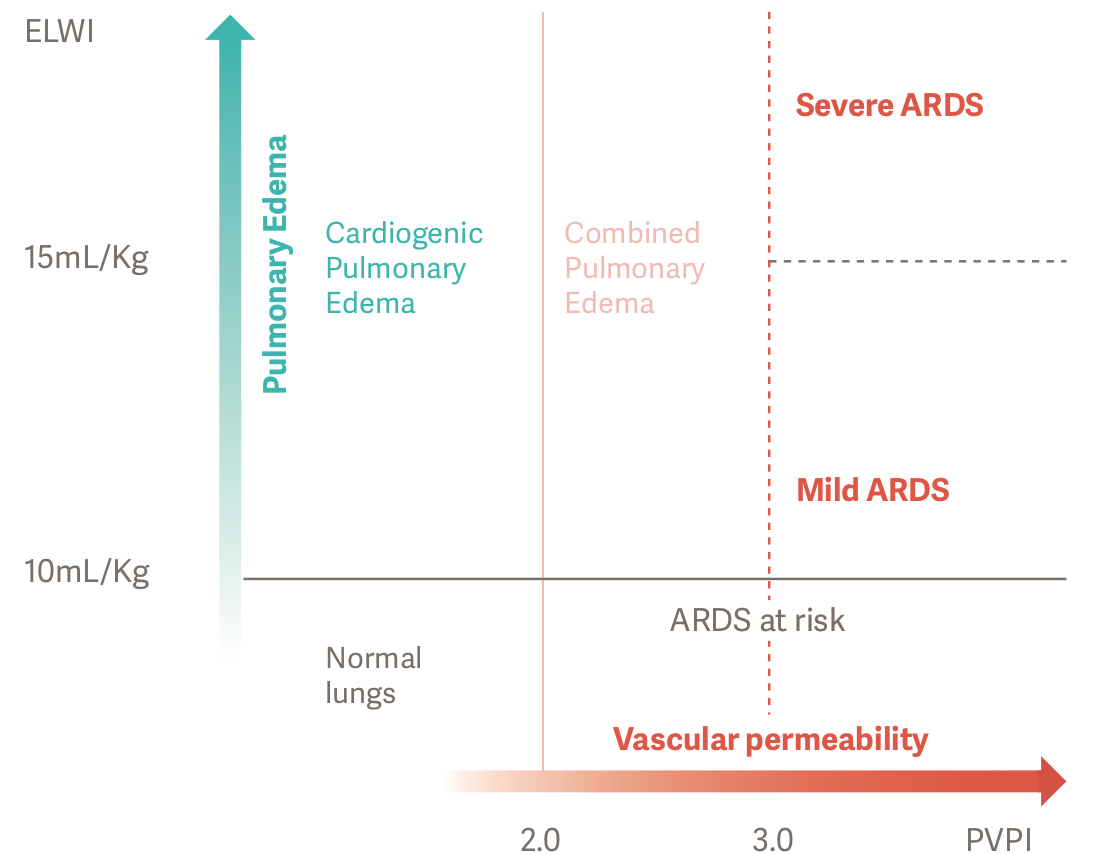
Accurate and objective diagnoses can be made for ARDS patients using ELWI and PVPI. PVPI more than 3 with ELWI above 10 ml/kg represents increased permeability pulmonary edema, or ARDS.[2]
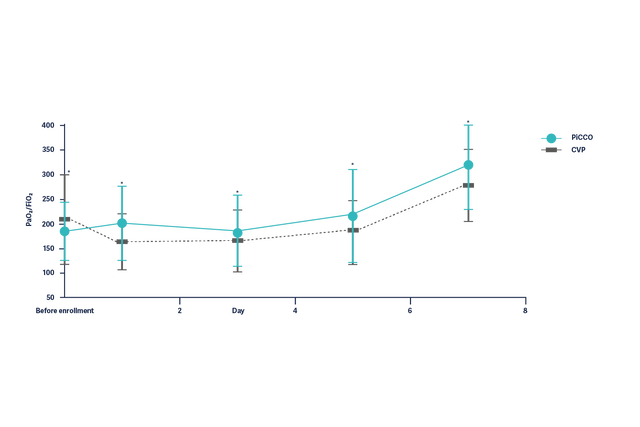
ARDS management based on PiCCO improves outcome
In the context of ARDS, studies suggest that management based on protocols including ELWI measurements is safe, leads to a lower cumulative fluid balance, improves ICU mortality, and reduces the duration of mechanical ventilation, of ICU stay and treatment costs.[10]
Improvement of the oxygenation (PaO2/FiO2) in ARDS patients over 7 days is significantly better in patients with hemodynamic management based on PiCCO parameters.