Why low-flow anesthesia matters for patients and the planet.
As early as 1924, R.M. Waters published an article in Anesthesia & Analgesia highlighting the benefits of using a rebreathing system in anesthesia: improved economy, convenience, and patient welfare [1]. Nearly a century later, these benefits are still true, and with today’s focus on sustainability, low-flow anesthesia also protects the welfare of our planet.
Low-flow anesthesia offers pulmonary, economic and environmental benefits
In low-flow anesthesia, the rebreathing system uses a fresh gas flow (FGF) lower than the patient’s alveolar ventilation. This technique uses less anesthetic agents than conventional systems, emits less gas into the atmosphere, and improves the flow dynamics of inhaled air. Low flow is generally characterized by a fresh gas flow of less than 1.0 L/min. In minimal flow, the FGF is decreased to 0.5 L/min.
Should we move to low- or minimal-flow anesthesia?
Reducing the fresh gas flow has several benefits:
|
|
Economy |
Agent expenditure accounts for a large part of the total cost of ownership of anesthesia machines. Reducing the anesthetic agent consumption in your operating room (OR) will have a positive impact on your overall hospital expenditure.
|
|
Environmental impact |
With low-flow anesthesia, a reduced amount of anesthetic gas is released into the atmosphere, lowering the environmental impact of fluorinated agents and nitrous oxide. This contributes to decreased ozone depletion and reduced greenhouse gas emissions.
|
|
Patient comfort and safety |
Low FGF improves the flow dynamics of inhaled gases, increases mucociliary clearance, maintains body temperature and reduces water loss.
|
|
OR staff safety |
With less unused surplus gas discharged into the atmosphere, the concentration of anesthesia gas in the OR is greatly reduced. This minimizes occupational risk for OR staff.
Simply low-flow anesthesia
Safe. Sustainable. Smart.
This new clinical booklet provides a step-by-step guide to performing low- and minimal-flow anesthesia with the Flow Family. It combines scientific background with practical instructions to support safe and confident use in daily practice.
Inside, you’ll find:
- Clear explanations of the low-flow technique.
- Practical guidance for applying it with Flow Family machines.
- Insights on safety, sustainability, and economic benefits.
Because sustainable, smart anesthesia isn’t just the future: it is something we can start today, one breath at a time.

What are potential risks of low-flow anesthesia?
Hypoxic mixtures
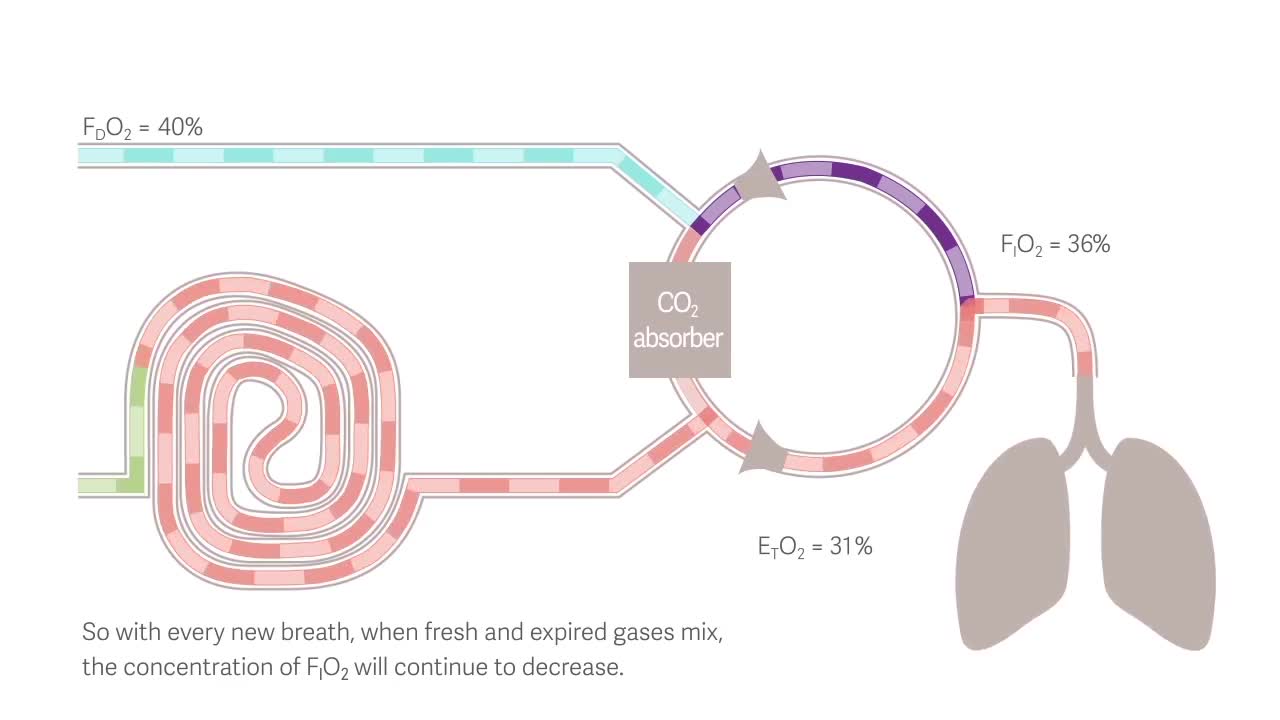
The formation of hypoxic mixtures are one of the greatest risk of using low-flow anesthesia. Reducing fresh gas flow in a rebreathing circle system results in a difference between the delivered O2 concentration(FD) at the common gas outlet and the inspired O2 (FIO2). Consequently, FIO2 becomes lower than the fraction of delivered oxygen (FDO2). This may not always be sufficiently recognized, and if settings are not adjusted, hypoxic mixtures can develop. An active inspired hypoxic guard has been shown to prevent the formation of hypoxic mixtures. [2]
Inadequate depth of anesthesia
During low-flow anesthesia there is a risk for inadequate anesthetic gas concentration. Rebreathing may cause the inhaled concentration to differ from what the anesthesia provider sets, leading to a perceived loss of control. The set levels of O2 and anesthetic agents may not match the inspired ones. Additionally, frequent adjustments to vaporizers, oxygen concentration, and fresh gas flow are needed, which can be demanding, especially during induction. Automated target control solves this by directly aiming for the desired end-expired anesthetic concentration (EtAA), reducing under-dosing and eliminating issues linked to low fresh gas flows. An automatic gas control (AGC) system removes the need for continuous manual adjustments of FGF, FiO2, and EtAA. Targeting FiO2 directly will help avoid hypoxia. Targeting EtAA at the desired speed will reduce the risk of under- or overdosing. [3]